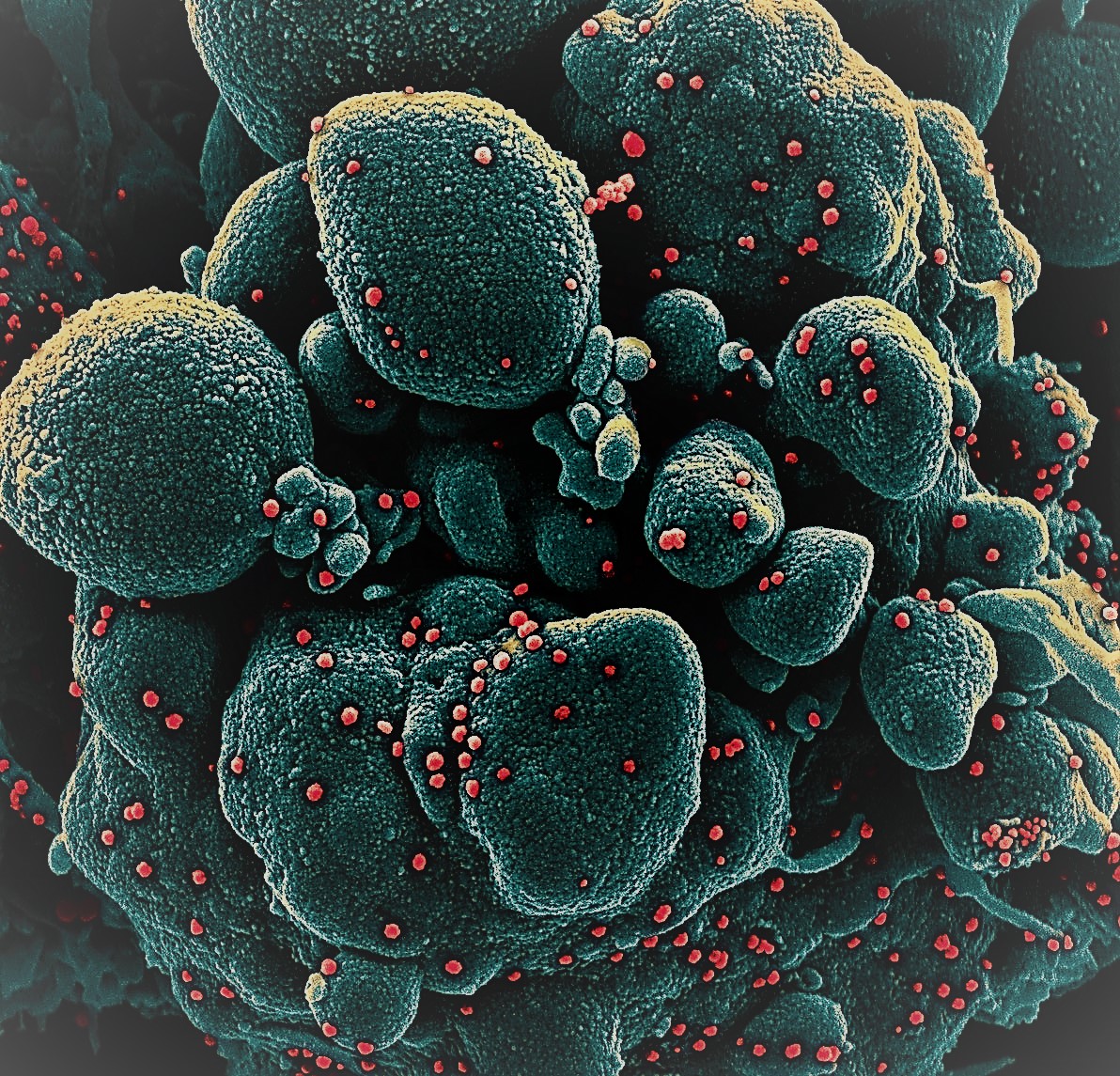
Calu-3 cells were identified as a suitable model system for the investigation of innate immune responses to SARS-CoV-2 infection in vitro in this work, which is consistent with numerous prior publications. Tese adenocarcinoma-derived lung epithelial cells exhibited critical RNA- and DNA-sensing pathway proteins, reacted to type I IFN stimulation, and were infected with SARS-CoV-2 in high numbers.
SARS-CoV-2 also stimulated transcription of type I and III IFN genes, as well as pro-inflammatory cytokines, in these cells. A549, HCT116, and THP1 cells were not permissive to SARS-CoV-2 infection and did not upregulate antiviral cytokines in response to the virus, as were the other cell lines studied. Other studies have found that A549 and THP1 cells are incapable of supporting viral entry and/or replication, most likely due to a lack of expression of the viral entry receptor ACE2.
Furthermore, it has recently been reported that high baseline RIG-I levels in cells like A549 hinder SARSCoV-2 replication. This could be due to reduced binding of the viral polymerase to viral RNA that is occupied by RIG-I, rather than IFN induction.
Surprisingly, the authors found large quantities of viral RNA in HEK293 and Huh7 cells but no activation of an IFN or cytokine response. It's been proposed that HEK293 cells express enough ACE2 to allow for viral entrance and beginning replication. However, the infection appears to remain dormant, with no significant progeny virus produced.
Why don't HEK293 cells respond to SARS-CoV-2 replication by inducing antiviral cytokines through transcription? The research team discovered that the MDA5 protein is undetectable in HEK293 cells at baseline, which could explain why SARS-CoV-2 isn't detected in these cells. Huh7 cells have been found to be viral replication-friendly. A proteomics-based technique recently discovered activation of the type I IFN system in Huh7 cells 48 hours after infection but not 24 hours after infection32. This suggests that IFN induction in Huh7 cells is delayed, which could explain our results at the 24h timepoint.
Other coronaviruses, such mouse hepatitis virus, produce MDA5-dependent type I IFN responses. The team now showed that the type I and III IFN responses to SARS-CoV-2 are dependent on the RNA sensor MDA5, its downstream adaptor MAVS, and the transcription factor IRF3 utilizing both shRNA-mediated knockdown and CRISPR/Cas9 genetic ablation. RIG-I was found to be mainly unnecessary for the antiviral cytokine response in Calu-3 cells. Other manuscripts revealed that MDA5 and its adaptor MAVS recognize SARS-CoV-2 infection while ours was being written. In Calu-3 cells, siRNA-mediated knockdown and/or genetic ablation were reported in three of the studies.
Another study reported that both MDA5 and RIG-I sense SARS-CoV-2 infection in Calu-3 cells, and that elevation of the pro-inflammatory cytokine IL6 was uncoupled from MDA5, but dependent on RIG-I and MAVS21, in contrast to these three findings and our results.
These findings were publish in Nature "Scientific Reports". This work used a siRNA knockdown technique; whether this or other technical factors are to blame for the discrepancy between these results and what the team and others describe needs to be seen. After transfection into human lung fibroblasts, total RNA isolated from SARS-CoV-2-infected Vero E6 cells activated MDA5, but not RIG-I, according to another study.
Interestingly, a different study used a similar experimental technique and found that type I IFN transcriptional upregulation after transfection of RNA from infected cells was dependent on RIG-I rather than MDA536. It would be fascinating to compare the different reporter cells utilized by Liu et al. and Wu et al. for RNA transfection side by side.
Surprisingly, their findings revealed that the MDA5-MAVS signaling pathway was not required for transcriptional activation of the inflammatory cytokines TNF and IL6. Tese cytokines are usually induced by the transcription factor NF-B, which is activated downstream of MAVS37 but can also be triggered by other PRRs such TLRs. TLR3, a transmembrane receptor found in endosomes and on the cell surface, recognises dsRNA and triggers a type I IFN response mediated by IRF3 and a pro-inflammatory response mediated by NF-B. TLR3 mutations are linked to illness severity in patients, implying that TLR3 plays a role in SARSCoV-2 response. Furthermore, when PRRs recognize damage-associated molecular patterns generated during infection, pro-inflammatory cytokines can be triggered.
Sensing mitochondrial DNA released into the cytosol in Dengue virus-infected cells has been demonstrated to activate cGAS and STING in this way. Indeed, it has been postulated that in response to SARS-CoV-2, the STING pathway causes NF-B activation and TNF production. The reduction of STING lowered, but did not eliminate, the TNF response to SARS-CoV-2 in our study.
However, because some residual STING protein was found in the targeted cells, it's possible that cytosolic DNA sensing by cGAS/STING increases TNF production in response to SARS-CoV-2 infection. In addition, Yin et al. found that the receptors LGP2 and NOD1 are necessary for the type I IFN response to SARS-CoV-2 in Calu-3 cells, in addition to MDA5-MAVS. LGP2 is an RLR that may operate to increase MDA5-mediated reactions, whereas NOD1 has just been discovered to aid RLR activation. NOD1 recognizes bacterial peptidoglycans and sends a signal to NF-B, which causes inflammatory cytokines to be produced. Furthermore, peptidoglycan-free pathogens, such as viruses, as well as ER stress, can cause NOD proteins to become activated.
The inflammatory cytokine response we saw in Calu-3 cells could have been caused by NOD signaling and/or other mechanisms. Taken together, the non-IFN pro-inflammatory cytokine responses they noticed the result of activation of PRRs other than MDA5.
Finally, the research team detected overexpression of MxA protein, which is encoded by an ISG, in infected cell populations using fow cytometry. This backed up our RT-qPCR findings, which showed upregulation of various ISG mRNAs in response to infection. They were able to distinguish infected cells from uninfected bystander cells in the same sample by staining for the viral nucleocapsid protein (N).
In comparison to infected cells, bystander cells showed a more significant induction of MxA. It's possible that viral infection interfered with IFN receptor signaling. Proteins in the IFNAR signaling cascade have been identified as targets of specific SARSCoV-2 proteins in previous research. Tis contains the viral ORF6, which suppresses STAT1 nuclear translocation and ISG promoter activation.
SARS-CoV-2 has also been demonstrated to suppress IFNAR1, JAK1, and TYK2 protein production, all of which are implicated in IFN receptor signaling. SARS-CoV encodes viral proteins that interfere with the type I IFN system, similar to SARS-CoV-2. ORF3a from SARS-CoV, for example, directly targets IFNAR, and NSP1 suppresses host gene expression to reduce STAT1 phosphorylation and IFNAR signaling. As a result, SARS-CoV-2 is expected to have additional proteins that inhibit IFN receptor signaling. These findings back with the theory that SARS-CoV-2 suppresses the type I IFN response, lowering host immunity and promoting virus spread.
the team showed that SARS-CoV-2 infection activates MDA5, which is required for type I and III IFN production in Calu-3 cells, along with its downstream signaling partners MAVS and IRF3. MDA5 was not required for the infection-induced pro-inflammatory cytokine response.







0 Comments
Feedback will be Appreciated